Published: June 6, 2017
Health TAPESTRY, a program developed at McMaster University to help older adults stay out of emergency rooms and be more mobile, is expanding to six Ontario communities this fall.
Led by the Department of Family Medicine, Health TAPESTRY is a unique approach to health care delivery that connects volunteers, communities, technology and interprofessional health care teams.
The program is receiving a $3 million boost to expand, with half the funds from the Ontario Ministry of Health and Long-Term Care, and half from Hamilton businessman David Braley.
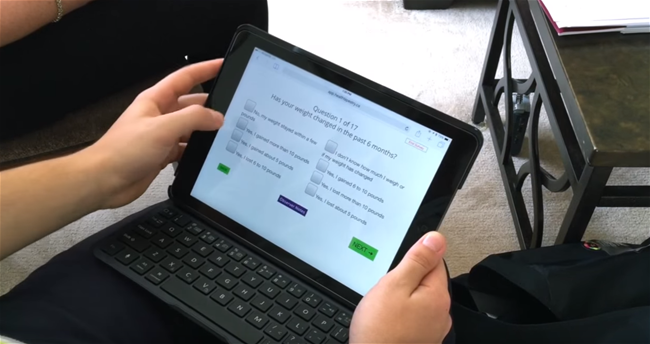
In Health TAPESTRY, trained volunteers visit clients at their homes to talk with them about the factors that are important to their health and life. During these visits, volunteers use a specialized computer app to gather this information and send it digitally to the client’s health care team. With this information, the health care team develops a plan to help address any health issues and goals with the client.
“Our government is committed to supporting Ontarians who want to stay in the comfort of their own home for as long as possible,” said Dr. Eric Hoskins, minister of health and long-term care.
“Connecting community and health resources locally, which Health TAPESTRY is doing, is a key step in providing the care they need closer to home. This community program is an exciting and innovative initiative.”
“The Health TAPESTRY program is a cost-effective way to improve individual health care,” said Dr. David Price, professor and chair of family medicine at McMaster.
“It is part of our department’s focus on improving systems of care so that they better fit the needs of our communities in ways that work for individual people.”
Dr. Doug Oliver, medical director at the McMaster Family Practice in Hamilton, added: “The life and health information volunteers gather by visiting and talking to people at home is invaluable for extending the care our interprofessional team provides to our community.”
The Health TAPESTRY program was developed with partners across Canada and piloted with six populations in six provinces through a $6.5 million grant from the Government of Canada and an additional $2 million contributed by the Government of Ontario, Labarge Optimal Aging Initiative, and the McMaster Family Health Organization.

