The new Juravinski gift will support research projects that are related to COVID-19 and brain health.
Published: ​​April 3, 2020
Thanks to the Juravinski Research Institute and the gift from Charles and Margaret Juravinski, leading experts from Hamilton Health Sciences, McMaster University and St. Joseph’s Healthcare Hamilton have funding to support the following eight collaborative research projects.
COVID-19 Research
N95 STUDY, COVID-19
What is it? A short-term study that will determine whether N95 respirators or medical masks are the best option for health-care providers caring for COVID-19 patients. N95 respirators are designed to protect the wearer from inhaling small airborne particles, while medical masks prevent facial contact with large droplets. Medical masks are less expensive and more readily available.
Why does it matter? This study is of critical value in informing the use of personal protective equipment for healthcare workers. There is serious concern about a shortage of N95 respirators because of COVID-19. There’s also concern that compliance with using N95 respirators could decrease over time because they have been associated with headaches and discomfort.
Leading health organizations disagree on which option is best, with the World Health Organization and the Public Health Agency of Canada (PHAC) recommending medical masks for the routine care of patients with COVID-19. They recommend N95 respirators for aerosol generating procedures only.
How does it work? In the multi-centre randomized controlled trial, nurses will be randomized to either use a medical mask or N95 respirator when providing care for patients with fever and respiratory illness.
Who’s doing it? The lead investigator is Mark Loeb, Michael G. DeGroote Chair in Infectious Diseases; Professor, Pathology and Molecular Medicine, McMaster University.
IMPACT OF A PANDEMIC ON HOSPITAL EMERGENCY DEPARTMENTS, CRITICAL AND INTENSIVE CARE UNITS, AND STAFF.
What is it? A three-part study cataloguing the activity of Hamilton Health Sciences Emergency Departments (EDs) for the duration of the pandemic. Insights from data will inform ED staffing and prediction of infection spread among health-care workers, and will help to better identify risks to them. As well, it will lead to better staff protection and patient care in hospitals, and will inform future hospital pandemic planning on a national level.
Why does it matter? There is a dearth of health-care research focused on pandemics, in part because of the logistical challenges faced by operationalizing such research. Given the potential for exponential growth in population infection, there are concerns that hospital systems will become saturated with critically ill patients, meaning that health care will be rationed, impacting not only those with COVID-19 but also patients who present to hospital with unrelated life-threatening health conditions.
How does it work? There are three parts to this study:
1. A registry to inform the Hamilton Health Sciences ED staff and senior leadership about patient activity during the pandemic, and a report of the frequency of COVID-19 infection and quarantine among the staff — to provide information about the local impact of the pandemic on both patient care and ED operations.
2. A medical-records review detailing the clinical outcomes of patients diagnosed with COVID-19, who are managed in the ED, to contribute to a national program of research by the Canadian Association of Emergency Physicians.
3. A national study on the effects of the pandemic on emergency physician work patterns, work challenges and health (both physical and mental health).
Who’s doing it? The lead investigator is Dr. Kerstin de Wit, Assistant Professor, Department of Medicine, Hamilton Health Sciences.
COVID-19 RAPID HIGH-THROUGHPUT AND NOVEL SAMPLING, EXTRACTION AND DETECTION SYSTEMS
What is it? A way to automate and ultimately speed up diagnostic testing protocols for SARS-CoV-2, the viral pathogen responsible for the COVID-19 pandemic, by using robotics. The screening process not only tests for coronaviruses, but simultaneously for a series of respiratory pathogens such as influenza A and B.
Why does it matter? The team of researchers quickly mobilized in the early days of the pandemic to become among the first to develop this test. Since mid-March, clinical labs have used the test, allowing for the identification of infected individuals much sooner, enabling appropriate quarantine procedures to be put in place in an effort to prevent the further spread of COVID-19.
How does it work? The research team designed multiple assays to detect the emerging viral pathogen, then provided them to the clinical laboratory for integration into a multiplex Pathogen Panel that allows simultaneous testing with the eight other common tests in their viral respiratory pathogen panel, and validated it with real specimens.
Next steps include acquiring robotics technology to rapidly test high volumes of samples, addressing the worldwide shortage of transportation for swabs and specimens, and implementing a test that can look at multiple targets within the virus.
Who’s doing it? The lead investigators are Dr. Marek Smieja, Chief, Hamilton Regional Laboratory Medicine Program; Head Section of Virology; and Dr. David Bulir, St. Joseph’s Healthcare Hamilton.
CANADIAN LONGITUDINAL STUDY ON AGING (CLSA): BUILDING COVID-19 PLATFORM FOR RESEARCH IN CANADA
What is it? The CLSA is Canada’s first comprehensive, population-based, and sustainably funded research platform, an ongoing longitudinal cohort study of 50,000 people ages 45 to 85.
Its COVID-19 platform will provide researchers with rapid access to a vast amount of high-quality biological, health, economic, environmental or psychosocial data, to address urgent health questions and to meet current and future health-care needs.
Why does it matter? Researchers can use the CLSA’s rich data to assess which factors appear to protect against or increase the risk of developing symptoms.
The data will offer insights that lead to better prevention and management of the pandemic, as well as the development of public-health programs and research into the mental-health and long-term consequences of the pandemic as people age.
How does it work? The CLSA’s COVID-19 platform will collect weekly and monthly data from its participants to gain a comprehensive picture of the spread and effect of the pandemic.
As well, existing CLSA data offers unique opportunities to understand why some individuals develop severe disease while others remain asymptomatic despite being infected by the virus, which will lead to better prevention and management strategies.
Who’s doing it? The lead investigators are Parminder Raina (Scientific director, McMaster Institute for Research on Aging) and Mark Loeb, (HHSC), Cynthia Balion (HHSC & St. Joseph’s Healthcare Hamilton), Marek Smieja (HRLMP), Lauren Griffith, Laura Anderson, and Dawn Bowdish.
COVID-19 BIOBANK
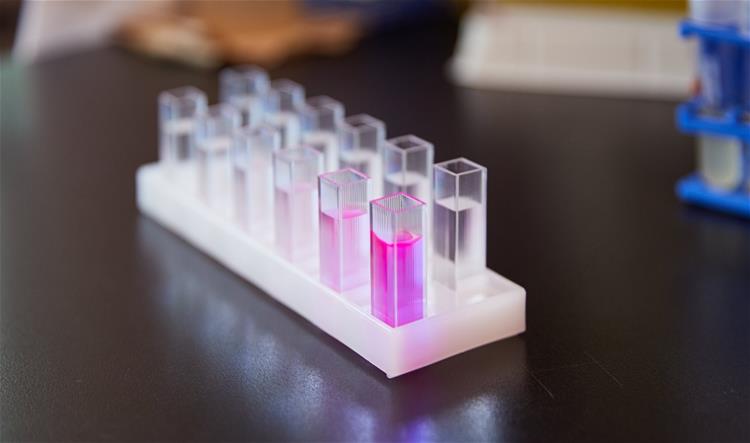
What is it? A biobank is a type of repository for storing human biological samples — an important resource in medical research.
Why does it matter? There needs to be a pathway for collecting samples during the COVID-19 crisis in Hamilton.
How does it work? Hamilton Health Sciences (HHS) has one of the largest biobanks in the country. HHS and other local cohorts will work together to accumulate and store samples for patients exposed or infected with COVID-19 in Hamilton for use in various studies by a variety of researchers across the three institutions.
To read more about Charles and Margaret Juravinski’s $3.3 million gift for COVID-19 and brain health research, please see this article on the Daily News, or read their remarkable letter to the community.
This article was first published on Brighter World. For all funded projects, please read the original article.

